Our story
We founded Leva in 2019 in the backdrop of significant change in the world of chronic pain.
Treatment guidelines were being undone. GPs stopped prescribing long-term ‘painkillers’ for persistent pain. Cannabis-based medication was legalised for specific uses where other treatments had failed. The emerging pandemic was about to unleash stress on the healthcare system and wait times like never before.
Today, 12m adults in the UK live with significant persistent pain. At least 500,000 are still prescribed high strength ‘painkillers’ that are unlikely to be doing much good. Waiting times are persistently long. Despite promising evidence and worldwide change, small numbers of people are prescribed cannabis-based medication.
If you’re one of the 12m people or someone who cares for them, then we’re here to help you find sustainable pain relief without unpleasant side effects.
We call it finding pain-life balance.
Our approach
We combine 1-to-1 support from your own team of pain specialists, science-backed tools to create lasting change and cannabis-based medicine.
Our team are known for their compassionate care for complex conditions, especially those often unrecognised and overlooked.
Between them they’ve run NHS pain clinics, been elected leaders of leading pain institutions and helped write the NICE guidelines on chronic pain.

How we're different
We fill the space between the NHS and cannabis ‘access’ clinics. Understanding why requires a short explanation.
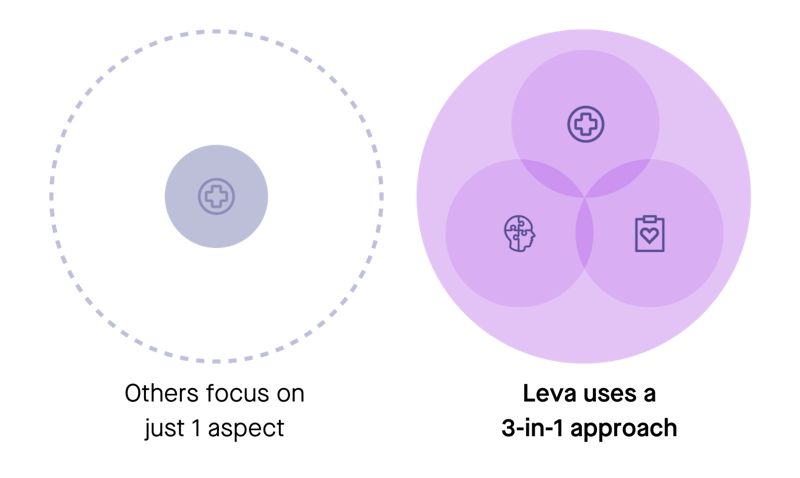
Almost 50 years ago a scientific paper was published proposing that we need a new approach to healthcare: a 3-in-1 approach (’biopsychosocial’) and not just the legacy, singular approach (’biomedical’).
To illustrate how groundbreaking this approach was in healthcare, the paper has been cited more times than the one introducing DNA to the world, and even Einstein’s paper on special relativity!
But because not all doctors and health professionals are familiar with it, some still use the legacy model that's less effective for supporting people with chronic pain.
This is part of the reason why you may have been made to feel like your pain is in your head when you can’t see a physical cause on an x-ray. And it’s one of the factors that went into the decision to stop prescribing opioids for chronic pain.
The 3-in-1 approach treats pain holistically for the best chance of success. This model celebrates the fact that we’re each complex individuals, and not machines.
Why this matters
Despite promising data and historic shifts in legal status across the world, prescribing cannabis-based medication alone for pain may only be of limited help.
If not treated as a stepping stone and holistically, there’s a risk that for many it’ll be a case of swapping prescription ‘painkillers’ for prescription cannabis - an expensive commitment.
Instead, we prescribe cannabis-based medication within a wider 3-in-1 approach. It’s like the difference between temporarily treating the symptoms, and addressing the root cause.
We care about quality care, and we care about giving you the best chance of finding pain-life balance - sustainable and lasting pain relief without unpleasant side effects.
Our credentials

We're the first fully-online pain specialist to be regulated by the CQC. We've been scored "Outstanding" for being Well-Led.

We're contracted by a number of NHS trusts to provide both self-management tools and clinician-led care for chronic pain patients.

We're one of a small number of hand-selected partners Boots offer in their Health Hub.

Named in "25 Ones to Watch" by Healthcare UK (Department for International Trade and NHS England).
Other notable awards and events
Department of International Trade's #Beyond100 Digital Health companies in 2022
Highly commended finalist for Tech Nation Rising Stars 3.0 - Diversity & Inclusion – Leading the Way Award 2021
London & Partners' Business Growth Programme 2020, supported by the Mayor of London
NHS Clinical Entrepreneur Programme 2021
Selected to present at Royal College of Physician's (RCP) Medicine 2021


Meet our pain specialists
Scroll to meet the team




